The discovery the world could not stomach
Andre Lo describes the troubled journey to a treatment for peptic ulcer disease
The medical world used to think that peptic ulcer disease was primarily caused by chronic stress, too much stomach acid or lifestyle habits like eating spicy food. This condition, which involved having open sores in the lining of the stomach, first part of the small intestine or lower oesophagus, was often chronic, excruciating and debilitating. In life-threatening cases, such as if the ulcers bled or became perforated, drastic surgery could be required to remove part of the digestive tract. Such an operation could leave the patient as a ‘gastric cripple’ – having to live with unwanted side effects such as appetite loss and deteriorating health. Thankfully, such stories are seldom heard of nowadays, due to the pioneering efforts of two Australian doctors: Barry Marshall and Robin Warren.
In 1981, Barry Marshall was completing his internal medicine fellowship at the Royal Perth Hospital, seven years after graduating from his medical degree at the University of Western Sydney. It was in June of that year that he would join the gastroenterology division of the hospital and meet Robin Warren, a senior pathologist more than a decade older than him. Warren had observed two years earlier that Helicobacter pylori, a corkscrew-shaped bacterium, was only found in stomach biopsies associated with gastritis (stomach inflammation). Because Marshall was recommended to pursue a clinical research project each year as part of his training, he decided to study the bacteria further with Warren.
They received one year of funding to in 1982 to look for the bacteria, but initially failed to culture anything from biopsies. It turned out that the cultures were thrown away after two days – the standard procedure for growing germs from throat swabs – but as it turned out, H. pylori was slow-growing. In the end, they found that the bacterium was only found in patients who had gastritis or ulcers, and inferred that H. pylori had a significant role in those conditions. But such a hypothesis was met with much scepticism from gastroenterologists. To them, the concept of a pathogen causing ulcers was like saying that pigs might fly. Unable to show how the bacteria acted in lab mice, rats or pigs (as it only affects primates), and bugged by the fact that severely ill patients were sent to undergo disabling surgeries instead of having their ulcers simply treated by antibiotics, Marshall thus took the drastic step of infecting himself with H. pylori.
Thus, on June 12, 1984, Marshall consumed H. pylori cultured from a patient, expecting to develop gastritis and possibly an ulcer in a few years. But very soon, he was feeling ill and vomiting every morning. An endoscopy after ten days, showed inflammation and damage in the lining of his stomach. It was obvious then, that H. pylori was the cause of gastritis. The results of his dangerous self-experimentation was published a year later, and with more research supporting the role of H. pylori in peptic ulcers and gastritis, their controversial theory was soon accepted by the World Congress of Gastroenterology, the National Institute of Health and the World Health Organisation.
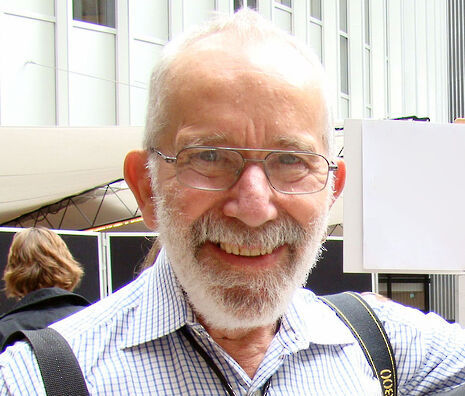
Marshall and Warren would later win the Nobel Prize in Physiology or Medicine in 2005 for their work. While Warren has since retired from medicine, Marshall went on to develop diagnostic tests for H. pylori and is still conducting research as the Professor of Clinical Microbiology at the University of Western Australia.
Maybe I am biased because I too hail from a sunburnt country. But I find their tale – a relentless pursuit by two then relatively unknown Australians to prove their convictions – truly inspiring. In doing so, Barry Marshall and Robin Warren remind us that we must keep an open mind, even when the truth may be hard to digest.
 News / Caius mourns its tree-mendous loss23 December 2025
News / Caius mourns its tree-mendous loss23 December 2025 News / Clare Hall spent over £500k opposing busway 24 December 2025
News / Clare Hall spent over £500k opposing busway 24 December 2025 Comment / The ‘class’ of Cambridge24 December 2025
Comment / The ‘class’ of Cambridge24 December 2025 Comment / Yes, I’m brown – but I have more important things to say22 December 2025
Comment / Yes, I’m brown – but I have more important things to say22 December 2025 Interviews / Politics, your own way: Tilly Middlehurst on speaking out21 December 2025
Interviews / Politics, your own way: Tilly Middlehurst on speaking out21 December 2025









