Curing cancer in the 21st century
Research into cancer has been going on for over a century. Why has it been taking so long to find a cure?

Cancer is one of the leading causes of death worldwide. According to the WHO, about 1 in 6 deaths are caused by cancer. Researchers around the world are racing to find a cure for the deadly disease – but why is it taking so long? And are we any closer to a cure than we were since Nixon declared a ‘War on Cancer’ in the 70s?
Despite there being no cure, if the disease is diagnosed at an early stage and then adequately treated, survival rates have risen substantially for many types of cancers. Average five-year survival rates for both breast and prostate cancers in the UK is over 80%, not to mention the far higher survival rates for tumours that are detected early on. Notable exceptions include cancers of the pancreas, liver, and lung. Nevertheless, all-cancer five-year survival has dramatically increased, for example in the US, from 50.3% in the 70s to 67% in the early 2000s. In this way, current treatments and managing relapse has allowed many people to lead long, successful lives and “beat cancer.”
We group cancer into one big category, but, in reality, the symptoms and clinical manifestations of different cancers are very unique. Particularly in the cases of metastases (cancers that spread from one part of the body to another), scientists are looking into how to restrict or stop that process. The initial localised tumour itself often does not cause quite as much damage. Therefore tumours that do not invade surrounding tissues are called ‘benign’, while those that do are referred to as ‘malignant’. It is metastasis that largely contributes to cancer deaths - as the tumour invades vital tissues, their functions are impaired, such as the liver, kidneys, or lungs.
Other major factors contributing to cancer mortality are the compromised immune system in cancer patients, and the wasting away of tissues. What is curious about all these metastatic mechanisms is that many of them seem to mimic the very ones that are vital in the formation of human tissue in an embryo. A major process underlying this is the epithelial to mesenchymal transition (EMT), that allows stationary cells to become motile and invasive, similar to the process that happens inside the early embryo.
This is one of the many ‘hallmarks’ of cancer, formulated in a seminal Cell paper by Douglas Hanahan and Robert Weinberg. These hallmarks include cancer cells evading being killed by the body, being self-sufficient in growing and responding to growth signals, evading growth suppressors, activating metastasis, dividing uncontrollably and making new blood vessels. Scientists are targeting every one of these mechanisms to try and figure out a way to restrain the disease and keep it in its localised target area.
Targeting one ‘hallmark’ of tumours does not guarantee success as these evolve new evasion strategies
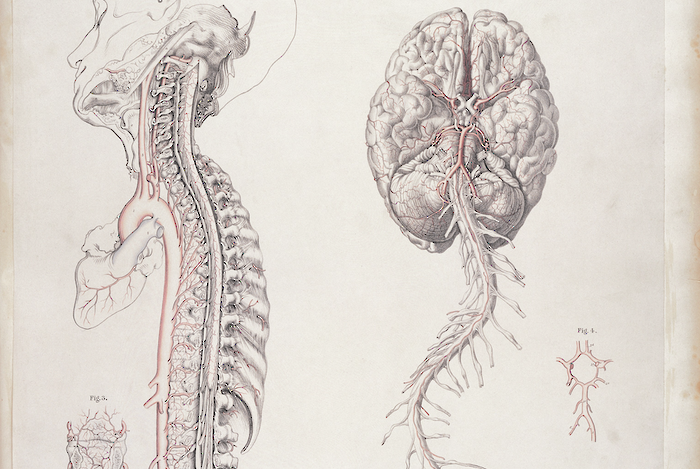
Another ‘hallmark’ currently being researched is the role of angiogenesis, the growth of new blood vessels. For the tumour to spread, it needs oxygen and nutrients to survive. Therefore, the growth of a blood vessel network is very important. As solid tumours grow, the existing blood circulation is insufficient to supply it, thus creating a low oxygen area within its core.
This hypoxic area thus releases pro-angiogenic signals. Several blockers of receptors involved in angiogenesis have been developed, with quite varying success rates. The major issue that remains, is cancers developing quite ingenious ways of gaining access to blood in the body. This observation is clearly something that cancer researchers can target to attempt to stop a cancer from spreading any further and limit its growth.
A further ‘hallmark’ of cancers is their ability to evade immune system surveillance and produce growth promoting inflammation. Usually, the immune system is very effective at killing tumours. So-called ‘natural killer cells’ are able to recognise tumour cells and destroy these. An early example of immunotherapy for cancer is the drug rituximab, an antibody which specifically targets white blood cells, and is thus used in lymphomas (as well as autoimmune diseases). A prominent example of a recent advance in fighting cancer is the gene engineering of immune cells. CRISPR-Cas9 gene editing has allowed us to engineer T cells, part of the adaptive immune system which can recognise cells that are infected by pathogens and kill these.
Usually, T cells rely on other immune cells to ‘present’ them with antigens of pathogens, so that these can identify what cells are infected (depending on whether they have a compatible T cell receptor) and destroy them. Now, with gene editing, these recognition receptors can synthetically be inserted into T cells, so they can recognise tumours expressing these and kill them. There are currently over 300 clinical trials, attempting to develop this form of therapy for several types of cancer. A major issue here is the potential immune response of the body to this treatment, as well as cancer evolving and no longer expressing the antigen the therapy is developed against.
Each and every stage in the oncogenic and metastatic process needs to be studied to find out if there are potential treatments. It is this very complexity in the formation and spread of cancer that makes it so challenging for scientists. Targeting one ‘hallmark’ of tumours does not guarantee success as these evolve new evasion strategies. Further, it is difficult to do so without affecting healthy bodily cells. The struggle against cancer continues, from the laboratory bench to the hospital bedside. Hopefully it will be a struggle of the past very soon.
 Features / Should I stay or should I go? Cambridge students and alumni reflect on how their memories stay with them15 December 2025
Features / Should I stay or should I go? Cambridge students and alumni reflect on how their memories stay with them15 December 2025 News / Cambridge study finds students learn better with notes than AI13 December 2025
News / Cambridge study finds students learn better with notes than AI13 December 2025 News / Dons warn PM about Vet School closure16 December 2025
News / Dons warn PM about Vet School closure16 December 2025 News / News In Brief: Michaelmas marriages, monogamous mammals, and messaging manipulation15 December 2025
News / News In Brief: Michaelmas marriages, monogamous mammals, and messaging manipulation15 December 2025 Comment / The magic of an eight-week term15 December 2025
Comment / The magic of an eight-week term15 December 2025