Repairing a highway: how can we fix spinal cord injury?
The functional sophistication of the spinal cord can have devastating consequences. Will modern scientific developments replicate its functions?
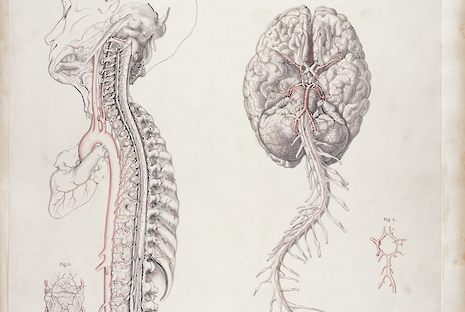
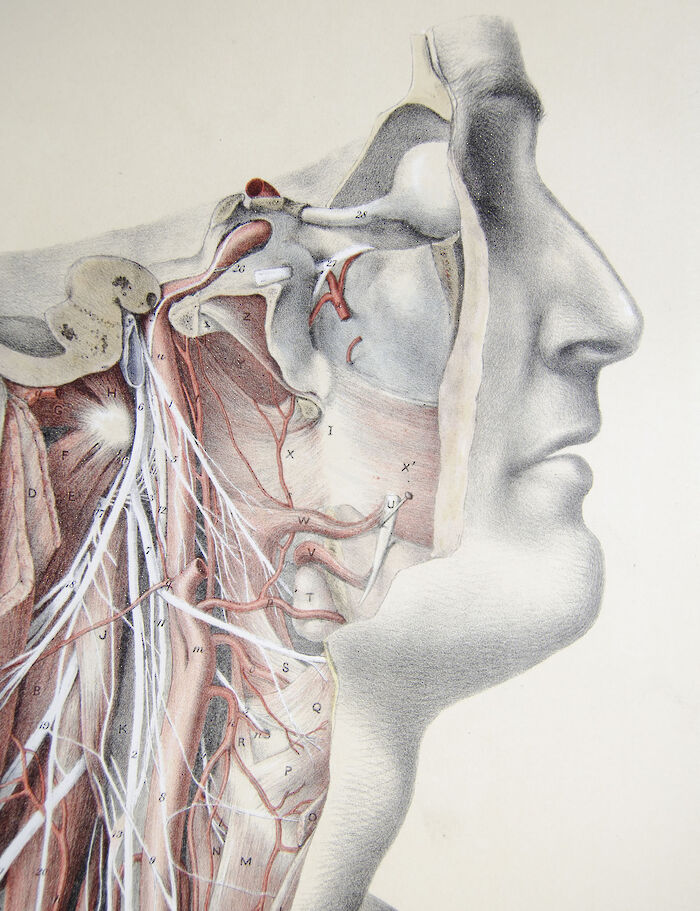
The “central nervous system” delicately orchestrates the complex concerto of our mental and physical faculties, from perception through to action and all the intermediary processes in-between. Such functional sophistication is disturbed in spinal cord injury, which can have devastating short-term and long-term consequences, determined by the level and severity of the injury.
The estimated incidence of spinal cord injury is around half a million people year worldwide, mostly affecting the young and elderly. The consequences of these injuries cannot be overstated, with people with spinal cord injury two to five times more likely to die prematurely.
Survivors struggle to attend school and work due to lasting debilitating conditions. These range from the primary impact of the injury leading to sensory and motor impairments and paraplegia, to secondary effects such as chronic pain, infections and depression and even psychosocial barriers leading to ostracism and exclusion.
Rehabilitation must therefore take a multi-faceted approach to maximise functioning, physical & mental wellbeing and community integration.
Neurobiologists have started to tackle the challenge of spinal cord injury with research aiming to rebuild the spinal cord.When the central nervous system is injured, it will respond by walling off the injured site with a “glial scar” and embedding this area with molecules that inhibit regeneration.
Repairing spinal cord injury therefore requires the alteration of regenerative potential. This is being explored through studies which graft supportive glial cells to the injured area and the development of biomaterial polymers which can bridge gaps in the spinal cord.
The most recent advancement in this field has used grafts of neural progenitor cells (stem cells committed to acquiring neuronal identity). These cells demonstrate the ability to extend their axons over large distances as they differentiate, whilst assuming appropriate cell fates (sensory/motor) according to the original spatial blueprint of the spinal cord anatomy. It remains to be shown whether such an approach can be extended from animal models to the human paradigm, and how the extent of functional recovery compares with other approaches.
Taking a different approach, neuro-engineers have been producing brain-machine and neural interfaces that can bypass injured neural areas to restore connectivity. These brain-machine interfaces are made up of a micro-electrode array implanted in the area of the brain where the command for voluntary movement is generated - the motor cortex. This records neural activity from the brain’s surface directly.
The recordings of the brain’s activity can then be reverse-engineered to decode the intended movement and programmed to produce the desired limb movement. This could be by controlling a robotic arm, or even an “exoskeleton”, as has recently been published in the Lancet Neurology.
The major advancement of this 65 kg robotic exoskeleton suit is the ability to activate all four limbs, whereas previous technologies that could produce movement in only one limb. The study participant trialling the novel exoskeleton was able to walk a considerable distance: around 145 metres, taking 480 steps.
These technologies are still generally cumbersome. They require vigilant laboratory-based monitoring by neurophysiologists and engineers.
Walking requires ceiling-mounted support since the complex neural mechanisms that enable us to walk upright are not fully understood
Moreover, the movement capabilities are still relatively primitive: walking requires ceiling-mounted support since the complex neural mechanisms permitting balance and equilibrium that enable us to walk upright have not been fully understood. Testing of the upper limb has also still been limited to simple reaching tasks. These do not yet capture the complexity of fine motor control such as intricate finger movements that the native nervous system is able to accomplish.
Many factors complicate our interpretation of signals from the brain. These include the chaotic behaviour (non-linearity) of signals from neuronal ensembles, and the low signal: noise ratio recorded.
In the future, engineers may be able to produce sustainable, durable, and fully-implantable stimulation systems that eliminate the need to don and doff components, and the development of software algorithms that allow more complex and simultaneous limb movements to be generated.
In addition, neurorehabilitation experts have been developing new methods to restore function in the nervous system, by promoting plasticity mechanisms intrinsic to the central nervous system. A recent study in Nature describes how a study participant with thoracic spine injury undertook epidural stimulation alongside numerous (113) intensive rehabilitation sessions, and gained the ability to walk a short distance (<100 metres) with relative independence from harness support and trainer assistance. This method involves a fully implantable system surgically placed in the epidural space and offers the convenience of usability in the home environment. The premise centres around “neuromodulation” of the spinal circuitry with epidural stimulation, through activation of previously dormant connections between neurons.
However, this is likely to be only effective for a subset of spinal cord injuries in which some functional redundancy is spared. Moreover, electrical stimulation systems have the general drawback of causing non-specific, widespread neural activation, and repetitive electrical stimulation may fatigue the targeted muscle fibres.
Given the multi-faceted nature of the problems posed by spinal cord injury, teams of experts in neurobiology, neuro-engineering and neurorehabilitation have racked their brains to come to a solution. These interventions have so far proven relatively promising, but are not yet practical, since the originally tetraplegic individual is still unable to walk for long distances or without assistance.
Nevertheless, they are a step in the right direction, and may pave the way towards achieving relative independence in activities of daily living. Perhaps it is likely that a combinatorial approach may represent “the science of the future to change … this harsh decree"of regenerative failure in the central nervous system, as memorably declared by Santiago Ramon y Cajal.
 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / Gov grants £36m to Cambridge supercomputer17 February 2026
News / Gov grants £36m to Cambridge supercomputer17 February 2026 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026 News / CUCA members attend Reform rally in London20 February 2026
News / CUCA members attend Reform rally in London20 February 2026 News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026
News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026