Excluding women in science can be fatal
Joyce Mau expounds on the importance of having female subjects in medical research

We’ve all heard of “Woman in STEM” – an iconic phrase used to describe a woman pursuing a career in science, technology, engineering, or mathematics. A cheeky reinterpretation of the phrase could flip it around and reinvent its definition: are women being sufficiently included, as research subjects, in scientific studies?
“Are women being sufficiently included, as research subjects, in scientific studies?”
A study conducted 10 years ago found that biological females were excluded from most biomedical research, based on fears that female hormonal variation would complicate findings. In 2019, this phenomenon was examined again: while there was a 21% uptick in the inclusion of females, the proportion of studies that analysed research results by sex did not improve. When studies lack a sex-focused analysis, we assume that findings can be applied to both biological males and females. This is dangerous and operates on a blanket disregard for the significant differences in biology and behaviour between both sexes. In reality, sex and gender are major determinants of health, and intersect with each other to affect patterns of disease and injury.
While this exclusion seems nonsensical in this day and age, a deep dive into the historical backdrop of women’s roles (or lack thereof) in medicine and society could explain why this has become the norm. For much of documented history, women have been excluded from medical and scientific knowledge production: in On the Generation of Animals, the Greek philosopher Aristotle characterised females as mutilated males (even though during the early development of a foetus, all foetal genitalia are the same and phenotypically female). Over the centuries, since men predominantly led the healthcare system, these systems were mostly catered to men – breakthrough discoveries in healthcare matters concerning biological females, such as endometriosis and even the best positions for childbearing, have only occurred in the last 200 years. Endometriosis, a chronic and incredibly painful gynaecological condition has been linked and misdiagnosed as “hysteria” in the past. Women who have endometriosis were characterised as unstable, gender deviant, unable to bear children, and therefore “hysteric”. This is but the tip of the iceberg.
A large study in 2018 reported that women have fewer risk factors for post-operative mortality than men and are less likely to experience complications overall. Yet, they found that women fare worse after cardiac and vascular surgery with a heightened risk of further strokes. Similarly, Ambien and other sleeping pills are examples of drugs with markedly different effects on women and men. These pills are recommended to be taken at least eight hours before one attempts to drive – however, since women metabolise the drug more slowly, they can still be too drowsy to drive eight hours after taking it. Eventually, the Food and Drug Administration cut the dose for women in half.
“Early heart attack signs were missed in 78% of women”
Furthermore, women and men describe symptoms of heart attacks differently. While men tend to describe cardiac arrest as crushing chest pain, women are more likely to report subtle abdominal pain or chest pressure, which means that they are less likely to be referred for aggressive diagnostic tests in a timely manner. Early heart attack signs were missed in 78% of women despite heart attacks being more deadly to them: those who have one are more likely to die or have a second heart attack compared to men. Yet, two thirds of clinical heart attack research is based on male physiology.
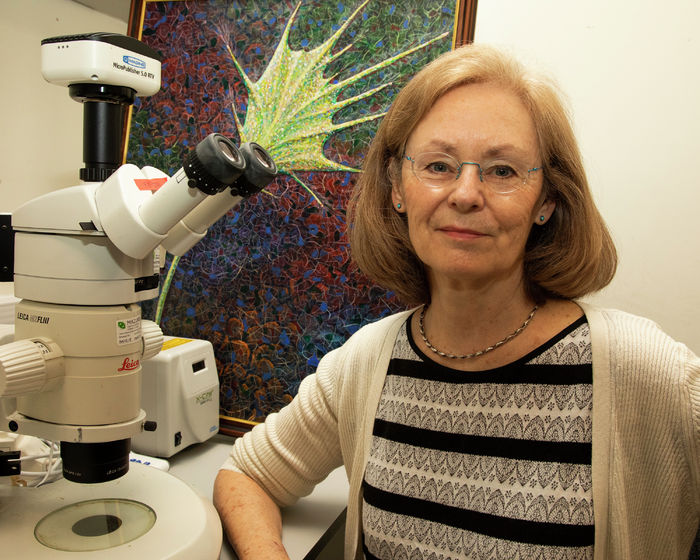
However, not all hope is lost. Medical researchers and practitioners are increasingly aware of the differences between biological men and women. A research team funded by the Canadian Institute of Heart Research and led by the University of Toronto’s Cindi Morshead discovered that the drug metformin, widely prescribed for diabetes, promotes repair in female brains but not in males, through sex-focused research. Their research benefits both men and women, preventing ineffective treatment for men, and promoting effective treatment for women. Various mechanisms, such as legislation, regulation, policies and guidelines have also been used to push for the inclusion of women in medical research.
We still have a long way to go in overcoming the challenges faced by a “Woman in STEM”. As Cambridge University continues to support the pursuit of STEM by women by nurturing female leaders in these industries, I have utmost faith they can and will ensure that women will never have to feel excluded from the healthcare system and beyond again.
 Comment / College rivalry should not become college snobbery30 January 2026
Comment / College rivalry should not become college snobbery30 January 2026 Features / Are you more yourself at Cambridge or away from it? 27 January 2026
Features / Are you more yourself at Cambridge or away from it? 27 January 2026 Science / Meet the Cambridge physicist who advocates for the humanities30 January 2026
Science / Meet the Cambridge physicist who advocates for the humanities30 January 2026 News / Cambridge study to identify premature babies needing extra educational support before school29 January 2026
News / Cambridge study to identify premature babies needing extra educational support before school29 January 2026 News / Vigil held for tenth anniversary of PhD student’s death28 January 2026
News / Vigil held for tenth anniversary of PhD student’s death28 January 2026