Cambridge Spotlight: New approaches to fighting cancer
In this next installment of Cambridge Spotlight, Izavel Lee explains how two teams of scientists from Cambridge have found different ways of treating this complex disease
A different kind of cancer drug
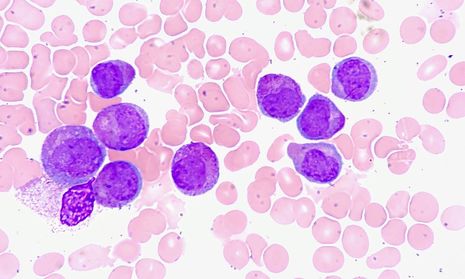
A team of researchers led by Professor Tony Kouzarides from the Milner Therapeutics Institute and the Gurdon Institute at the University of Cambridge have developed a new class of drug that could treat acute myeloid leukaemia (AML). AML is a cancer that usually affects myeloid cells, a type of cell which eventually transforms into white blood cells. However, in AML, the myeloid cells proliferate excessively and become unable to turn into white blood cells. Only around 20% of people in the UK diagnosed with AML will survive 5 years or more after their diagnosis.
In 2017, Professor Kouzarides and colleagues previously found that an enzyme, METTL3, is essential to supporting the growth of AML. METTL3 is involved in the process of converting DNA to RNA, an important step in producing proteins. When METTL3 is over-produced, certain types of proteins in the cell may be over-produced as well, resulting in AML. In their new study published this week in Nature, Professor Kouzarides and his team have showed that a drug called STM2457 can shut down the activity of this enzyme, and hence halt the development of AML.
“This is the beginning of a new era for cancer therapeutics”
To identify this drug, the team screened over 250,000 molecules for the potential to target METTL3. They then analyzed the drug for its ability to bind to METTL3, and tested it on human AML cells. The results were positive – STM2457 stopped the cancerous myeloid cells from proliferating, and they became able to turn into white blood cells normally.
Following this evaluation, the researchers investigated the effect of STM2457 on mice transplanted with human AML cells. Sometimes, drugs that seem to work well on cells in a petri dish may not perform to expectation when tested in living organisms. Fortunately, this was not the case for STM2457. In fact, when the mice were treated with STM2457 daily, they lived significantly longer than the control group of mice that were untreated. The AML cells did not proliferate as much, exactly the result that was obtained in cellular experiments. In addition, the mice suffered no toxic side-effects or effects on their body weight.
Besides developing a new drug for AML, the team has also shown for the first time that cancers can be treated by targeting this process of converting DNA to RNA. “Until now, no one has targeted this essential process as a way of fighting cancer. This is the beginning of a new era for cancer therapeutics,” said Professor Kouzarides.
Finding cancer’s weak spots
Cancer develops as a result of mutations in our DNA. Different patients may have different mutations in their DNA, even patients with the same kind of cancer, and this can change how effective different treatments are for each patient. For example, some cancer patients may have a type of mutation called mismatch repair deficiency (MMD) that affects their ability to repair certain kinds of DNA damage.
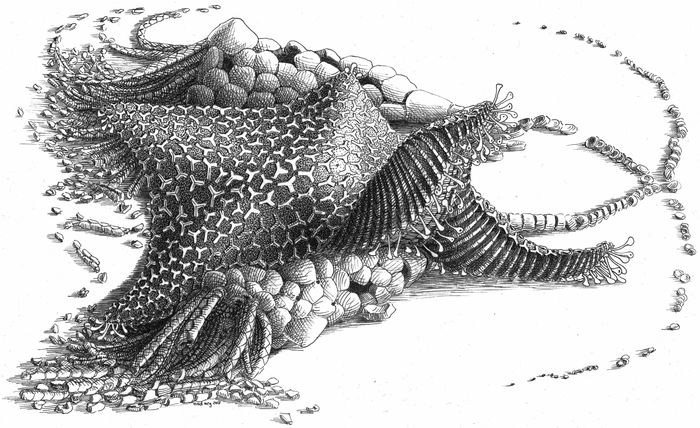
Now, a team of scientists led by Dr Serena Nik-Zainal from the MRC Cancer Unit at the University of Cambridge has developed an algorithm that can identify such cancers with MMD. Using the gene editing technology CRISPR-Cas9, the researchers deactivated various DNA repair genes in stem cells. As cells usually mutate as part of natural processes, deactivating these genes was expected to result in even more mutations. After growing these altered cells, they sequenced the cells’ genomes to identify the kinds of mutations that had occurred.
“Determining the right treatments for patients will give them the best chance of surviving their disease.”
It turned out that in cells with particularly important repair genes deactivated, the researchers could make out a distinctive pattern of mutations, termed a mutational signature. “When we knock out different DNA repair genes, we find a kind of fingerprint of that gene or pathway being erased. We can then use those fingerprints to figure out which repair pathways have stopped working in each person’s tumour,” explained Dr Nik-Zainal.
For example, the OGG1 gene is normally involved in fixing guanines that are damaged by oxygen. Guanine is one of four types of nucleotides alongside adenine, thymine, and cytosine, which are the building blocks of DNA. When it is deactivated, cells become unable to repair any damaged guanines, producing a specific pattern of guanines that are converted into thymines.
Using these findings, the team developed the algorithm MMRDetect that can identify cancers with MMD based on the mutational signatures in the genome of the patient. To train their algorithm, the researchers used DNA sequences from hundreds of colorectal cancer patients via the UK 100,000 Genomes Project (UK100kGP), run by Genomics England.
By identifying cancers with MMD, clinicians can recommend patients for treatment with immune checkpoint inhibitors (a type of immunotherapy drug), which are known to be effective in treating MMD cancers. There are now plans to run this algorithm on all cancer genomes that are obtained by Genomics England. Michelle Mitchell, Chief Executive of Cancer Research UK said, “Determining the right treatments for patients will give them the best chance of surviving their disease. Immunotherapy in particular can be powerful, but it doesn’t work on everyone, so figuring out how to tell when it will work is vital to making it the most useful treatment it can be.”
 News / University Council rescinds University Centre membership20 February 2026
News / University Council rescinds University Centre membership20 February 2026 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026 News / Union cancels event with Sri Lankan politician after Tamil societies express ‘profound outrage’20 February 2026
News / Union cancels event with Sri Lankan politician after Tamil societies express ‘profound outrage’20 February 2026 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / Caius students fail to pass Pride flag proposal20 February 2026
News / Caius students fail to pass Pride flag proposal20 February 2026