An Introduction to Vaccine Challenges: Part 4
Dr Hicham Bouabe goes into yet more depth on the challenges of vaccine research, including what happens when a virus mutates or a vaccine misfires.

In the previous parts of this series, we have so far discussed the challenges related to the vaccine formulation itself and to the route of its administration. In this part, we will go through the challenges imposed by viruses, the immune system, and experimental procedures.
Changes in the pathogen coating represent big challenge to vaccine development
Many pathogens, especially viruses, have the capability to change their antigens via mutations (called antigenic shift). Hence a vaccine against an antigen won’t be effective anymore against a target pathogen if it modifies its antigens. Therefore, constant updating of vaccine formulations is required.
This is, for example, the ongoing challenge in the case of influenza vaccines, of which composition is updated annually based on information gathered from the Global Influenza Surveillance and Response System (GISRS). In order to define the type of circulating influenza viruses, the GISRS collects and analyses influenza virus samples from around the world on an ongoing basis. Each year, the virus components of the vaccine designated for the coming influenza season might be changed to reflect the most frequent and recent circulating types of influenza viruses. Therefore, flu vaccination provides in most cases only a partial protection, at both individual and community levels.
The ultimate solution to overcome the issue of antigenic variation is to seek conserved antigens in target pathogens, which on one hand don’t undergo mutations, and on the other hand provide optimal immunogenicity in a vaccine formulation.
Immune response diversity in humans
There are many factors that determine variations of the immune system, including genetic background, type of nutrition, type of microbiota residing in the body, age, general health status, chronic diseases, infectious diseases history of each individual, etc.
A vaccine against a given pathogen needs to be developed for the whole community, but because of the immune system diversity, distinct types of immune response with different magnitude might be induced in individuals against the same antigen. A vaccine that induces an appropriate protective immune response in some people might induce only a weak non-protective immune response in other people. Alternatively, the vaccine might trigger misfire of the immune system in others, resulting in health-threatening inflammatory or autoimmune diseases.
Hence, there is a call to perform preclinical and clinical studies on animals and volunteers with broad immunological backgrounds in order to develop vaccines applicable for a broad spectrum of people with similarly diverse immune systems. Furthermore, the animal models used for preclinical research need to be revised, as discussed in the next section.
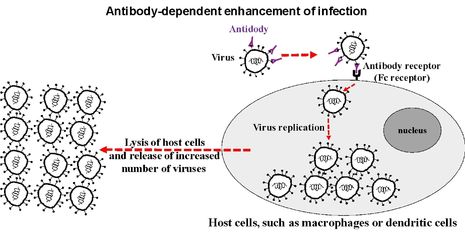
The risk of vaccine misfire: ‘antibody-induced enhancement’ of infectious diseases
An additional major obstacle to the development of successful vaccines against infectious microorganisms, is a phenomenon called ‘antibody-induced enhancement’ of infectious diseases (Taylor et al. Immunol Rev. 2015).
Vaccines against viruses are often formulated in a manner to stimulate the immune system to produce types of antibodies that recognise and block specifically surface proteins of the target viruses and thus inhibiting their entry into host cells, resulting in their neutralisation by the immune system. But, in some cases, ‘suboptimal’ types of antibodies are produced upon vaccination, which bind to the surface proteins of viruses, but instead of mediating their neutralisation, the antibodies facilitate the entry of the viruses into certain cells, such as macrophages and dendritic cells, through ‘antibody receptors’ (Fc receptors). Such antibodies help the virus to invade the cells, where they can replicate, and thus resulting in disease exacerbation.
For instance, an early epidemiological study from 1969 reported that the administration of a formalin-inactivated vaccine against the respiratory syncytial virus (RSV) resulted in high incidence of severe illness in 80% among vaccinated infants when they became naturally infected with RSV, compared to only 5% of the unvaccinated infants. The exacerbation of the disease was triggered by vaccine-induced antibodies against RSV surface proteins.
Misleading animal models for vaccine development
A very common animal model used in life science research, including vaccine development, is the mouse. However, its immune system shows fundamental differences to that of humans (Mestas & Hughes, J Immunol. 2004). Also the translation of experimental results in other animals, such as rats, rabbits, guinea pigs, ferrets, and nonhuman primates, to clinical studies in humans often fails.
“Several HIV vaccines that succeeded in animals failed in humans”
Furthermore, animal studies are conducted under well-controlled, sterile laboratory conditions. For instance, the animals chosen for a given study have the same genetic background and age, and haven’t experienced any previous disease and are kept in a sterile and uniform environment, eating the same food and so forth. In real life, however, humans are exposed to highly non-sterile environments, they experience different type of diseases including infectious diseases, have had several vaccinations, and they vary not only in respect to their genetic background, but in almost all aspects of their life, including nutrition, microbiota, age, immune response, weight and other variables.
These differences between the immune system of animal models and humans, and between the animal experimental conditions and the life conditions of humans, has often led to the failure of clinical trials, even if the candidate vaccines showed very promising results in animals.
A well-known example of unreliability of animal experiments is in HIV/AIDS vaccines. Several HIV vaccines that succeeded in animals, including non-human primates such as the chimpanzee, failed in humans (Aysha Akhtar, 2015).
The most recent HIV vaccine failure is the HVTN 702 clinical trial (NIH, News Releases from 03rd February 2020). In this trial, which began in 2016, vaccine formulations consisting of a live attenuated HIV vaccine (ALVAC-HIV) and a subunit HIV vaccine (subtype C gp120/MF59) were administered over a period of 18 months to 2694 volunteers in South Africa, 2689 volunteers received placebo. Subsequent analyses revealed that 129 HIV infections occurred among the vaccine recipients, and 123 HIV infections occurred among the placebo recipients, so the vaccine clearly doesn’t prevent HIV. The US National Institute of Allergy and Infectious Diseases (NIAID) announced in 2020 the end of the HVTN 702 clinical trial.
Thus, there is a call on one hand to discover/establish new animal models that show very similar susceptibility and immune response to infections and to vaccine formulations, like humans; and on the hand to increase, and at a very early stage during development processes of vaccines, the employment of – carefully and safely designed – experimental procedures in voluntary humans.
In the next and last part of this series, we will discuss the need of a ‘universal vaccine platform’ that would allow a very fast development of vaccines against pandemic and newly emerging pathogens.
 News / Union debates officer resigns after misconduct investigation9 March 2026
News / Union debates officer resigns after misconduct investigation9 March 2026 News / Man found guilty of murdering Cambridge language school student10 March 2026
News / Man found guilty of murdering Cambridge language school student10 March 2026 Features / The hidden harms of college stereotypes 10 March 2026
Features / The hidden harms of college stereotypes 10 March 2026 News / King’s Affair adds charge for half-off workers 11 March 2026
News / King’s Affair adds charge for half-off workers 11 March 2026 News / King’s faces backlash over formal ticket policy 7 March 2026
News / King’s faces backlash over formal ticket policy 7 March 2026









