This Week In COVID-19 Research: 5
Maria Izmirlieva summarises the major scientific breakthroughs in COVID-19 research including, but not limited to, risks of second coronavirus infections, efficacy of face masks, and R-values rising across the UK.
This last week will likely go down in history; it is marked by political turmoil, civil unrest, and the empowered resurgence of the BLM movement against ingrained, systematic oppression. More than ever, this is an unsettling yet critical period on a global landscape. Despite perhaps not being at the forefront of media attention, COVID-19 research into treatments, potential vaccines and epidemiological initiatives to minimise transmission, remains as crucial as ever.
The hydroxychloroquine saga continues
In the last few days a highly-influential paper, which led the World Health Organization (WHO) to suspend hydroxychloroquine and chloroquine trials, has been retracted. The Mehra et al. paper, published in the Lancet on 22 May, had questioned the safety and efficacy of hydroxychloroquine and chloroquine for the treatment of COVID-19. The peer-reviewed paper had relied on clinical data obtained from the little-known Surgisphere Corporation. Concerns were raised regarding the validity of the data, including an open letter from a number of researchers and an expression of concern published by the Lancet itself. Following the paper’s retraction, the WHO announced on 3 June that it will resume the temporarily paused hydroxychloroquine and chloroquine arms of the SOLIDARITY trials.
“The hydroxychloroquine group also reported a higher incidence of side effects”
However, the data validity problems may extend further: the New England Journal of Medicine (NEJM) has published its own editorial expression of concern in relation to other studies reliant on Surgisphere data, including one on the Angiotensin-converting (ACE) inhibitor and angiotensin-receptor blocker COVID-19 study.
Find the retracted paper here.
While the Mehra et al study may have been discredited, it is far from certain hydroxychloroquine will eventually demonstrate benefit in COVID-19 treatment. It failed to demonstrate usefulness as a prophylaxis in a study recently published in the NEJM. Boulware et al. of the University of Minnesota randomly assigned 821 people either hydroxychloroquine or placebo within four days of exposure to SARS-CoV-2. The results indicated no statistically significant difference between the two groups: 12% of the hydroxychloroquine group developed COVID-19 within 2 weeks, compared to 14% of the placebo group. The 107 participants who developed COVID-19 were diagnosed either using a PCR test or symptomatic criteria. The hydroxychloroquine group also reported a higher incidence of side effects, therefore the drug is likely to be of limited value.
Find the paper here.
Review into efficacy of face masks
The efficacy of face masks in reducing SARS-CoV-2 transmission has been a contentious topic, with certain countries mandating their use and the WHO being reluctant to recommend their use by the general public. A study in April in the Annals of Internal Medicine had questioned the efficacy of cotton and surgical masks, but this has since been retracted. This highly popular paper had concluded that such masks seemed ‘ineffective in preventing the dissemination of SARS-CoV-2’ from coughing by infected individuals.
“In England, use of face coverings becomes compulsory on public transport from 15 June”
On 1 June, the Lancet published a systematic review and meta-analysis evaluating the efficacy of face masks, eye protection and physical distancing in preventing person-to-person transmission of SARS-CoV-2. This incorporated 172 observational and 44 comparative studies across 16 countries and indicated that facemasks provided significant protection. Of the various face mask types, N95 respirators were shown to be most effective. The use of eye protection was associated with a 78% reduction in risk of transmission. Physical distancing of at least 1m also led to a large reduction in risk of 82%.
This systematic review has led the WHO to change its guidance on face mask usage on 5 June, with direct implications for society and public health. Those over 60 or with health issues should wear a medical-grade mask, whereas all others should wear a three-layer fabric mask. In England, use of face coverings becomes compulsory on public transport from 15 June; use of face masks by doctors becomes mandatory from the same date.

The retracted paper.
Find the new Lancet paper here.
Blood group may influence susceptibility to severe COVID-19 respiratory complications
Researchers from Oslo University Hospital have recently identified two human gene variants associated with an increased risk of respiratory failure as a complication of COVID-19 disease. This complication occurs in 10% of infected patients and is a crucial driver of mortality.
This research took the form of a genome-wide association study (GWAS), in which researchers attempted to find a correlation between DNA markers and the presence of a trait in an individual. This research involved the genome analysis of 1980 patients with severe COVID-19 with respiratory failure, and over 2000 controls without the disease. These individuals came from seven Italian and Spanish epicentres of the European pandemic.
“Their paper suggests that the R-value nationally is 0.9-1, with a risk of a rise in infections in certain regions.”
One of the variants found to be correlated with increased risk lies in the ABO blood group locus, the part of the genome which determines blood group. A follow-up analysis also revealed that those at highest risk of respiratory failure had A+ blood group. In contrast, individuals with type O blood appeared to be more protected. This result was true for both the whole cohort, as well as when it was subdivided into Italian and Spanish groups only. However, it is key to note that the study has not been peer-reviewed yet.
Find the full paper here.
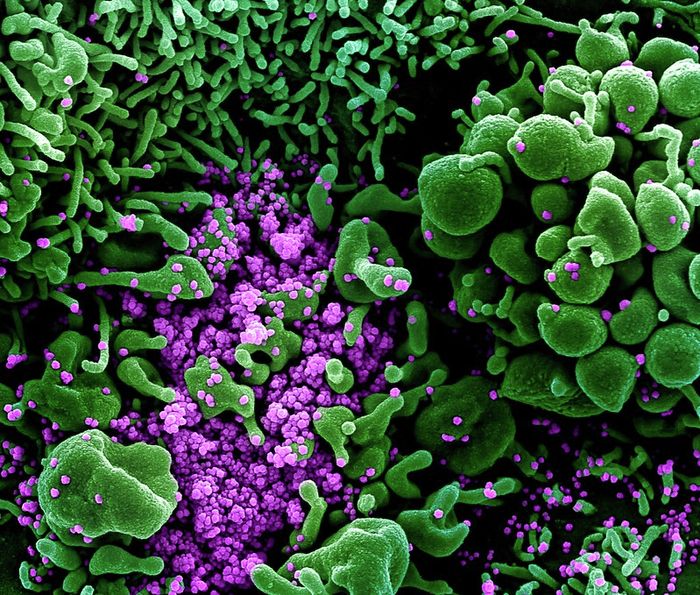
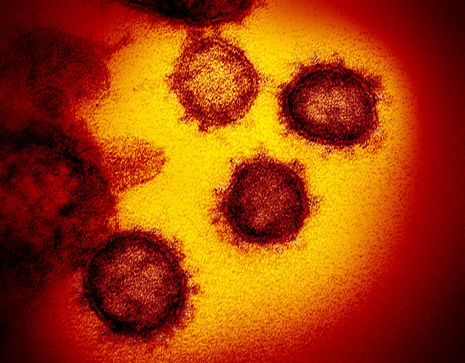
SARS-CoV-2 infection protects against reinfection in rhesus macaques
Our understanding of the immunopathogenesis of SARS-CoV-2 is critical for informing public health strategies and vaccine development. However, current knowledge of its protective immunity is limited; particularly, whether infection induces natural immunity which protects the individual on subsequent exposure.
To investigate this, researchers developed a rhesus macaque model and observed virologic, immunologic and pathologic features of SARS-CoV-2 infection on exposure and re-exposure. Specifically, they measured the viral loads in the upper and lower respiratory tracts, the cellular and humoral immune responses, and pathologic evidence of pneumonia. Following viral clearance, the rhesus macaques were re-exposed to SARS-CoV-2 and these features were measured. A comparison between primary and secondary infections revealed a drastic reduction in median viral loads, suggesting that SARS-CoV-2 induced protective immunity on re-challenge in non-human primates. Naturally, this does not provide conclusive evidence of long-lasting immunity in humans and further testing is required.
Find the full paper here.
Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19
Results of a recent randomised control trial involving convalescent plasma therapy were reported in the Journal of the American Medical Association (JAMA) this week. This therapy, which has already been the focus of several studies, involves using the plasma of individuals who have recently recovered from SARS-CoV-2 infection to treat patients with severe COVID-19. The study included 103 patients across seven medical centres in Wuhan, China, with severe and laboratory-confirmed COVID-19. Of these, 52 received convalescent plasma therapy in supplement to the standard treatment.
Although the results indicated no statistically significant improvement for patients using convalescent plasma therapy versus the control group, it is important to note that the study was terminated early and may have been underpowered due to a low sample size. Difficulties in recruiting patients with serious complications may have been difficult at the time the trial was conducted, given the success in controlling the outbreak in Wuhan.
Find the full paper here.
The R-value rises in England
A recent analysis from the London School of Hygiene and Tropical Medicine, providing modelling estimates of the R-value, suggests it is increasing. Their paper suggests that the R-value nationally is 0.9-1, with a risk of a rise in infections in certain regions. The R-value, known as the ‘effective reproduction number’, provides crucial information on a disease’s ability to spread. An R-value of 1 is equivalent to an infected individual transmitting the disease to 1 other individual on average before either recovering or dying. If the R-value exceeds 1, there will be exponential growth of the outbreak. Such information is critically important to policy makers, particularly in navigating an easing of lockdown restrictions.
Meanwhile, the government’s official estimates, based on Office of National Statistics data, suggest the R-value has declined and is currently between 0.7 and 1.
However, a prominent model, from Public Health England (PHE) experts and the University of Cambridge, estimates R stands at 1.01 for the north-west and 1 for the south-west. The government may find itself under pressure to reverse some of the lockdown easing for particular regions of the country if these findings are confirmed.
Find the paper here.
Model from Cambridge here.
 News / Union debates officer resigns after misconduct investigation9 March 2026
News / Union debates officer resigns after misconduct investigation9 March 2026 News / Man found guilty of murdering Cambridge language school student10 March 2026
News / Man found guilty of murdering Cambridge language school student10 March 2026 Features / The hidden harms of college stereotypes 10 March 2026
Features / The hidden harms of college stereotypes 10 March 2026 News / King’s Affair adds charge for half-off workers 11 March 2026
News / King’s Affair adds charge for half-off workers 11 March 2026 News / King’s faces backlash over formal ticket policy 7 March 2026
News / King’s faces backlash over formal ticket policy 7 March 2026