This Week In COVID-19 Research: 4
This week, Bartek Witek writes on the most recent advancements in COVID-19 science, covering possible new drugs, field-testing methods and more.
Studies continue at a faster rate than science has ever seen before on this novel coronavirus, SARS-CoV-2. Some questions have been raised, summarised in this article, as to the effect this haste has on the quality of science produced. Otherwise, this week we cover: novel field-testing methods for COVID-19 infection; an update on hydroxychloroquine; a review of numerous potential drugs, including remdesivir; ethical concerns regarding the treatment of non-COVID patients being delayed; and the potential link of COVID-19 to shingles and seizures.
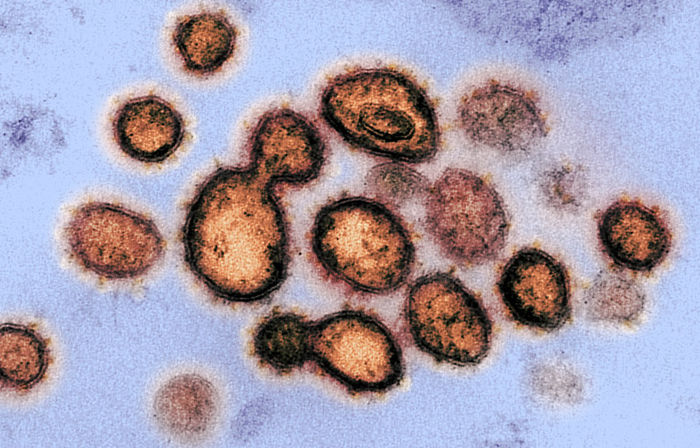
Field-testing of coronavirus
Currently, RT-(Q)PCR is a technique to detect the virus. This method relies on detecting viral RNA, requiring large, expensive and hard-to-operate machines. On the other hand, antibody tests can be used in the field but lack the same level of sensitivity and also take a long time to produce.
The proposed approach here is using something called a reverse transcription–enzymatic recombinase amplification (RT–ERA) reaction to create an ultra-sensitive, field-deployable testing method. It is a very similar technique to PCR (polymerase chain reaction, used commonly to amplify DNA samples) that detects the viral RNA but works at lower temperatures without large thermocycler machinery. In theory, RT-ERA can be done in a single test-tube.
To achieve this, they created a simple protocol. The reaction is carried out in a single tube, utilising a series of two water baths at 37/40C – no thermocycler needed! The products can quickly be detected by green fluorescence using blue light without uncovering the lid. This also reduces any possibility of contamination to improve the reliability, to hopefully measure even the smallest amounts of virus.
Taking it a step further, the researchers designed a ‘flow strip’ that could be used at home using only a thermos cup to detect the virus to a high degree of sensitivity, not even needing a water bath.
Study here.
Update on the study discrediting hydroxychloroquine
Last week, we mentioned the study that prompted the WHO to halt hydroxychloroquine trials as a treatment for COVID-19. An interesting development is being investigated by the Guardian. It was found the data used in the study was not available from the Australian clinical database and did not agree with local state data. This raises interesting questions about how the researchers got the data, indicating a lack of transparency in data sourcing. Mistakenly, data from an Asian hospital was included in the Australian dataset where obviously the two are not comparable. Some questions were also raised on the methods of statistical modelling employed. Please, however, note hydroxychloroquine is still currently not recommended as a safe and effective treatment, and the findings remain unchanged. Could the mad rush to find new treatments for COVID-19 be compromising the quality of the literature? As seen, any such study can have enormous implications on policy decisions, with the potential to save or end lives.
Remdesivir review
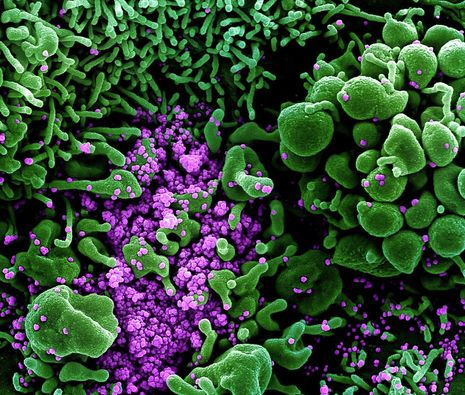
Hailed as a possible breakthrough drug originally designed to tackle Ebola, Remdesivir is facing its initial clinical tests after in vitro investigations summarised in this review.
Pharmacologically, Remdesivir is a nucleoside analogue (very similar to viral RNA) and inhibits viral replication. Emerging data suggests potent activity against COVID-19 and other coronaviruses, with potent viral inhibition seen in airway epithelial tissue in vitro. The possibility of resistance was investigated, with mutants showing reduced susceptibility to the drug in vitro but was associated with fitness costs elsewhere, resulting in the non-mutant virus outcompeting resistive strains.
Animal studies in rodents and rhesus monkeys showed positive outcomes. Less weight loss, lower viral load and reduced signs of disease were observed when administered before the infection. The same was observed when administered post infection but outcomes were less promising. It was important to note administration two days post infection did not improve outcomes, and the drug did not prevent mortality when a lethal dose of the virus was administered. Specifically, CoV-2 showed improvements in the lower respiratory tract but lesser improvements higher up. In humans, this could represent a transmission risk even following patient improvement.
Limited clinical data currently exist. Initial reports were plagued with poor experimental design and small sample sizes but showed little benefit in administering the drug post peak viral replication (when the disease has progressed to its worst). First randomised, double-blind, placebo control trials were published showing no significant difference in improvement time between Remedisvir and the placebo group. Earlier-stage patients (less than 10 days after symptoms) showed marginally better outcomes and interestingly showed no impact on the amount of virus.
The benefit is currently only seen as modest at best, with possible adverse effects including hypotension, liver enzyme abnormalities and renal impairment. The report highlights the need for more clinical trials and the limitations of using animal models as seen by more modest in vivo outcomes. Many patients are already supplied with the drug by doctors but are not included in trial data, highlighting the need to create infrastructure to include them to create larger samples. Only more clinical trials will show its real efficacy.
Study here.
Management of non-COVID patients during pandemic
A growing number of reviews are appearing about the treatment of other diseases during the pandemic. It is important to consider the effects of postponing key treatments, changes in consultation practices (i.e. cancer treatments) as well as new dangers presented to high-risk groups. Oncology councils are used to dealing with patients case-by-case but now face the need to consider wider measures due to the scale of the pandemic. As an example, there is an inverse relationship between treatment delays and survival rates with cancer, with recommendations drafted for Greek physicians with methods to reduce risk to patients and guidelines for treatment practices. Highlights include delays of up to 8 weeks for surgery on patients who have a 50% or higher curative rate, continuation with chemotherapy with additional safety precautions and limiting invasive diagnostic techniques. No clear recommendations exist for late-stage cancer patients, with most care being performed on a case-by-case basis. Returning to normality is just as important as finding a cure.
Study here.
COVID-19 could be associated with shingles and seizures
Herpes Zoster (more commonly known as shingles) may be added to the list of skin abnormalities reported with COVID-19 patients. Two patients were admitted into two independent clinics, symptomatic of shingles and reporting no COVID-19 symptoms but later developing respiratory problems. It is hypothesised that COVID-19 could infect white blood cells and kill them, leading to impaired responses to other viruses.
Study on Herpes Zoster association here.
COVID-19 may also be associated with acute seizures, also reported in two cases. The mechanism of neurological symptoms is unknown but possibly caused by the cortical irritation as the blood-brain barrier erodes and cytokine reactions caused by the viral infection.
Study on seizures here.
Ibuprofen and related drugs not yet recommended
A review investigated the possibility of using non-steroidal anti-inflammatory drugs (NSAIDs) as a treatment for the disease. Six trials were included in the analysis and found NSAIDs are effective at treating infections caused by influenza and rhinovirus (flu and cold) but no studies have been conducted on COVID-19. It is recommended to use substitutes as there is sparse data on the subject and only preliminary case reports and clinical experience available. In fact, it was found that ibuprofen may have exacerbated the condition of some patients.
Study here.
New kids on the block - more possible treatment candidates
New potential antiviral drugs are constantly being investigated. Researchers created a two-tiered drug screening system and applied it to FDA approved drugs. The screening system involved looking at the amount of virus present via antibody tests and judging cell viability. They looked at reduction in viral load in infected cells via plaque reduction assays in combination with time-of-drug-addition assays - introducing drugs at different stages of the disease. Screening 1528 FDA approved drugs and using these indicators, they found the following successful candidates: Cetilistat, diiodohydroxyquinoline, abiraterone acetate, and bexarotene. These exhibited potent in vitro anti-SARS-CoV-2 activity. The antiviral drugs we need could already exist and the work of these researchers puts forward ways we can quickly test them.
Study here.
 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / Gov grants £36m to Cambridge supercomputer17 February 2026
News / Gov grants £36m to Cambridge supercomputer17 February 2026 News / CUCA members attend Reform rally in London20 February 2026
News / CUCA members attend Reform rally in London20 February 2026 News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026
News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026