Remembering Ebola: two years on
Two years after the end of the West African Ebola epidemic, are we prepared for another outbreak?

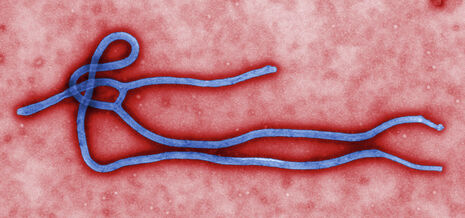
Nearly two years ago, the World Health Organisation (WHO) declared the end of the 2014 Ebola epidemic in West Africa. By then, the virus had infected 50 times more people than any previous Ebola outbreak.
Apocalypse averted, in other words.
Nonetheless, more than 11,000 people were killed before arguably outdated methods, such as isolating cases and quarantining the contacts of those diagnosed, put an end to the outbreak. Overall, inadequate health facilities, sub-standard infection control and a slow international response contributed to the most widespread outbreak of Ebola in history. The fact that in 2017 the word barely passes our lips begs the question: where do we currently stand in the war against of Ebola?
“What is the likelihood of a future Ebola outbreak? High, actually”
In the wake of the 2014 epidemic, a pharmaceutical marathon has ensued. Scientists in Russia and China have already licensed vaccines. Most recently, a vaccine touted as 100% effective, rVSV-ZEBOV, has been placed under review for use by the FDA in the USA. The genetic ‘spine’ of this vaccine is that of the vesicular stomatitis virus, which infects cattle but not humans. Spliced into the spine is the gene coding for the membrane protein of the Zaire strain of the Ebola virus that prompts the immune system to make antibodies against the pathogen, without the virus taking hold. It is suggested that in the event of another Ebola outbreak, the world might be able to turn to an emergency supply of this vaccine, currently available in a bank of 300,000 doses.
Yet, what is the likelihood of a future Ebola outbreak? High, actually. The virus is under evolutionary pressure to infect humans more readily. The A82V mutation, which alters the protein used by the virus to enter host cells, arose early in the 2014 epidemic and coincided with its acceleration. This makes sense, since studies show that the A82V mutation allows the Ebola virus to infect humans up to four times more efficiently than the ‘original’ strain.
A further exacerbating factor is urbanisation, which also contributed to the unleashing of HIV. According to the African Development Bank, the continent has had the world’s highest urban growth rate for 20 years, and the proportion of Africans living in cities will rise from 36% today to 60% by 2050. When it comes to infectious diseases, living in such close quarters can lead to disaster.
“Evidently, this is not only West Africa’s problem”
Alongside advances in vaccination, there are other ways in which we can prepare for a further Ebola outbreak. Pivotally, West Africa must strengthen its health infrastructure, in particular, with respect to hospital infection control and educating the public. Furthermore, surveillance could prove key to limiting future outbreaks. The 2014 Ebola crisis mobilised unprecedented financial assistance for West Africa: $400 million from the World Bank was directed towards an ambitious blueprint that revolves around the concept of public health surveillance. Each country in West Africa is to share surveillance data systematically, with a regional hub via a national coordinating institute. While this is planned to be fully staffed by early 2018, at the last report just 9 of the 15 countries had designated their national coordinating institute. It is crucial that a move is taken from words into action, so that future cases may be able to be detected and dealt with more quickly, and tragedy averted.
Evidently, this is not only West Africa’s problem. As an international community, we need to unite behind the broader aims of improving living conditions and sanitation, stabilising healthcare facilities, and promoting education if we are to curb future epidemics
 News / Report suggests Cambridge the hardest place to get a first in the country23 January 2026
News / Report suggests Cambridge the hardest place to get a first in the country23 January 2026 Comment / Cambridge has already become complacent on class23 January 2026
Comment / Cambridge has already become complacent on class23 January 2026 Comment / Gardies and Harvey’s are not the first, and they won’t be the last23 January 2026
Comment / Gardies and Harvey’s are not the first, and they won’t be the last23 January 2026 News / Students condemn ‘insidious’ Israel trip23 January 2026
News / Students condemn ‘insidious’ Israel trip23 January 2026 News / Cambridge ranks in the top ten for every subject area in 202623 January 2026
News / Cambridge ranks in the top ten for every subject area in 202623 January 2026









