Regenerative medicine: magic bullet or mirage?
In conversation with Anna Philpott, Professor of Oncology and member of the Cambridge Stem Cell Institute
The field of regenerative medicine has been viewed by many as a magic bullet in treating degenerative diseases, yet 25 years on from when the term was first used by Leland Kaiser in a publication about the future of healthcare, there have been virtually no instances of effective translation into the clinic. I spoke to Anna Philpott, Professor of Oncology and member of the Cambridge Stem Cell Institute, to discuss the advantages of the technology and the stumbling blocks of the field.
Philpott suggests that the field of regenerative medicine has two interpretations. One is “simulating your own endogenous ability to repair your tissues by understanding the normal mechanisms that contribute to repair” as well as “reactivating developmental processes.” The other more widely known approach is “producing cells or tissues outside the body and somehow managing to graft them into the appropriate place and integrate within your tissues.”
Increasingly a buzzword in discussions about the future of health, Philpott proposes that people underestimate the difficulty of the procedure: “You imagine I’ll be able to make some pancreatic beta cells and put them back in someone who has diabetes, and I’ll be able to cure their diabetes.” Yet the procedure faces many technical challenges: “You have to get cells plumbed into the appropriate place… [and] protect them from immune attack.” Additionally, she proposes that many misconceive claims about the external production of certain cell types: “The things you make outside the body never function in exactly the same ways as the things you make inside the body. So I think there’s a lot of hype that has yet to be realised.” Philpott reckons the former interpretation of regenerative medicine may be more effective, yet this faces its own set of problems when you “regenerate too much,” including producing “tumours or chronic inflammation…the last thing you want to do if you’re ageing.”
“We don’t know enough about normal biology to be able to bring about effective regenerative therapy”
Professor Anna Philpott
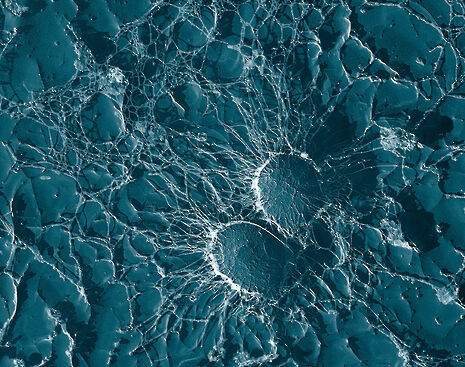
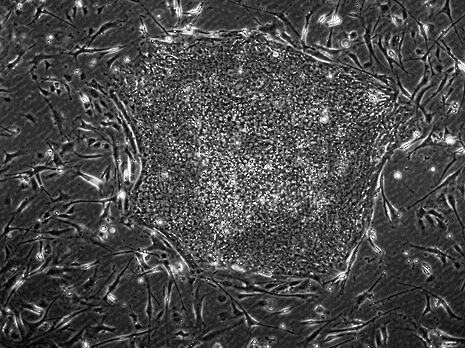
Translation into the clinic has seldom been achieved, even with many labs across the world working to provide novel treatments. Philpott says that “we don’t know enough about normal biology to be able to bring about effective regenerative therapy.” This she attributes in part to the fact that “developmental biology has fallen out of fashion over the last 30 years,” proposing that people don’t recognise that regenerative medicine is just “developmental biology in action.” Without a knowledge of how normal cells develop, whilst you can “superficially produce cells that look like the cells you want, they won’t behave like cells that you want.” This neglect of understanding normal biology she attributes to the genesis of the regenerative medicine field about 20 years ago, where researchers would “get some cells and would put a bit of this and a bit of that and a bit of the other growth factors and they’d find cells that beat, and they’d go ‘great I’ve made cardiac muscle.’” Now, people have started to add factors as they appear in the embryo and are getting much more “physiologically relevant” results. Yet these protocols face another challenge, namely the fact that they only produce immature cells: “it’s that final process of maturation that is missing from most protocols, and that really is a developmental process that we have yet to understand even at a fundamental level.”
Philpott proposes that the field needs to “see the bigger picture” in order to make progress. Developmental biology sees repeated patterns in regulation across seemingly disparate tissues. “In my lab, we work in neuroscience, we work in the pancreas, and we work in the gut, because we see that there are analogous mechanisms going on. It’s like nature re-uses the same module in different circumstances, because of course that’s the most evolutionarily efficient thing to do.” She attributes siloing into disciplines as one of the factors driving tunnel vision, suggesting that “physical scientists, or mathematicians, or people like that, are actually able to step back and look at the systems as a whole, as opposed to focussing too much on the molecular detail.” Whilst proposing that a focus on molecular detail has its place, Philpott says “maybe we’ve become side-tracked in the last few years because we’ve put too much emphasis on sequencing things.” So absorbed in the excitement around sequencing, people neglect the importance of the phenotype, she proposes. “The phenotype of cells depends on the sequence of the genes but also on how all of those things interact at the systems level, and you can’t get that information just by sequencing alone.” At the end of the day, it’s the phenotype that matters when treating disease: “In cancer biology for instance, it’s of course important to know the genotype, but it’s the phenotype that kills you.”
Besides technical issues, Philpott laments bad science in the field. She points to the case of Paolo Macchiarini at the Karolinska Institute who was widely reported to have undertaken risky first-in-human experiments using artificial tracheas to replace damaged organs without adequate pre-clinical studies to back up his approach. These lacklustre efforts can “set the field back by 10, 20, 30 years if there’s not sufficient regulation. And what regulation there is can vary enormously from country to country.”
“It won’t be available on the NHS or in other countries, it would only be available to the super-rich”
Professor Anna Philpott
Even though the field has had setbacks, Philpott envisages a gradual rolling-out of the procedure in selected tissues. She wouldn’t put a date on when we could all expect it — “it’s like saying when are we going to cure cancer” — but points to pigmented retinal epithelial regenerative therapy being carried out in London as a case of translation to the clinic already occurring. Whilst reducing the need for individualisation of the procedure, for example by having a “bank of enough cells with a good enough genetic match to do transplants, from which you generate tissues,” may reduce the cost of the procedure, the main challenge in translation is economics. “At least initially, it won’t be available on the NHS or in other countries, it would only be available to the super-rich, because it would cost so much.” Regenerating tissues within the body may cut costs further, she suggests, “but it may be less high-profile and take longer to develop.”
The issue of cost brings into question whether this magic bullet is really worth it: “If you use a lot of money on regenerative medicine then you won’t be using it in other areas.” In some cases, there may be cost savings: for example, inserting “immuno-privileged devices” with beta-cells into diabetics will be cheaper than present options, as “it costs such a lot of money over a lifetime to monitor and treat people with diabetes.” Yet for most cases, when, or indeed if, such treatments arrive, they may only be available to the rich with private healthcare. Further, Philpott suggests, there is a disconnect between the target market of the therapy and the optimal patient in which to use it: “regeneration is going to work better in young people but the biggest market is going to be old people who want to live much longer.”
In sum, regenerative medicine, despite its hype, faces numerous developmental, regulatory and economic challenges before it can be translated into the clinic. And even if regenerative medicine procedures are discovered that could be used in the clinic, it then raises the question for public health officials and governments as to whether they should be used. In the glare of the optimism of this field, we often forget that other, simpler procedures, or even basic public health, may be a much more ethical and effective use of resources
 News / Right-wing billionaire Peter Thiel gives ‘antichrist’ lecture in Cambridge6 February 2026
News / Right-wing billionaire Peter Thiel gives ‘antichrist’ lecture in Cambridge6 February 2026 News / John’s duped into £10m overspend6 February 2026
News / John’s duped into £10m overspend6 February 2026 News / Epstein contacted Cambridge academics about research funding6 February 2026
News / Epstein contacted Cambridge academics about research funding6 February 2026 News / Corpus FemSoc no longer named after man6 February 2026
News / Corpus FemSoc no longer named after man6 February 2026 News / Lucy Cav students go on rent strike over hot water issues6 February 2026
News / Lucy Cav students go on rent strike over hot water issues6 February 2026










