Antibiotic resistance: how do we manage the outbreak of ‘superbugs’?
With the capacity to use antibiotics comes a responsibility to manage the interaction between our doses and the bacteria we look to eliminate, argues Zi Ran Shen
Recently, a woman was killed by superbugs which resisted every available antibiotic – even colistin, an antibiotic with massive side effects used only in last resort situations. We are living in an era that no longer has a failsafe antibiotic. The emergence of antibiotic resistant bacteria was always a threat, but now it’s finally arrived.
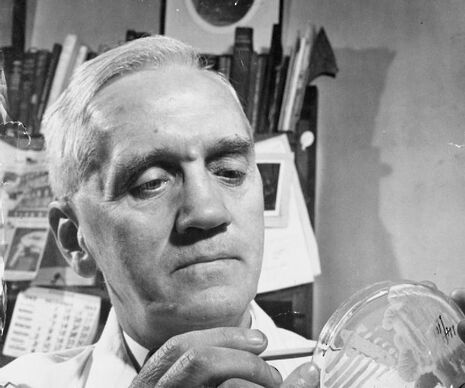
The story of antibiotics first began with a boy in a shipping office. Not having much money, Alexander Fleming was all but resigned to such a job for the foreseeable future. As it happened, he did not have to stay after receiving enough inheritance from his uncle. His brother, Tom, encouraged him to follow his footsteps in becoming a doctor.
During WWI, Fleming worked as a medic and saw many soldiers die from infected wounds. Back then, the only way to fight infections was to use antiseptics such as ethanol, iodine, and hydrogen peroxide. However, excessive use of antiseptics can worsen wounds as they slow the healing process.
When he returned home, he concentrated all efforts on finding an antibiotic which would revolutionise the medical landscape. After many years of very successful research but little progress on the antibiotic front, Fleming woke up to something most scientists would be irked to find – an agar plate contaminated with fungus. Fleming noted, however, that no bacteria were growing next to the fungus, and the further away the bacteria were the healthier they looked. He extracted the contaminating fungus and purified the incriminating substance he called ‘mould juice’, now known as penicillin.
The discovery of penicillin began a new era in medicine. Countless people were now prescribed a cheap and easy drug for what used to be a deadly problem. Got an inflammation? Have some antibiotics! Have a viral cold? Have some antibiotics! Just feeling malaise? Have some antibiotics! These drugs were prescribed left and right for minute discomforts that had little to do with bacteria.
Alongside the mass over-prescription of penicillin, many other antibiotics were discovered. And with the wealth of alternatives, humans for the first time felt invincible – we had slayed one of the four horsemen of the apocalypse.
“While we are gleefully popping antibiotics for every little illness, bacteria are plotting their resurgence.”
But the rosy glow of safety did not last. The first case of penicillin resistance was reported in the early 1950s, a mere 10 years after its introduction. One by one, our antibiotic protectors fell by the wayside. In 2007, we no longer had any antibiotic without resistance. The horseman has come back with a vengeance. Today, resistance is rising faster than ever due to improper use. While we are gleefully popping antibiotics for every little illness, bacteria are plotting their resurgence.
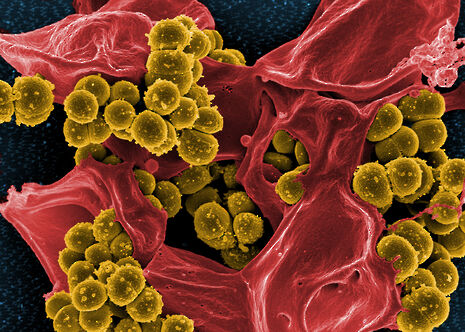
Bacteria who have picked up the ability to metabolise antibiotics can transfer such information to other bacteria through many means. Unlike higher order organisms, bacteria can absorb other bacterial genetic material from its surroundings. If a bacterium with antibiotic resistance dies, a new one can come along and pick up the gene conferring resistance easily and carry it on. The gene can then be replicated and passed along to others who need it to survive. Bacteria can easily latch onto travelling vessels and move to a new location to proliferate and amplify the gene of interest. Two living bacteria can also exchange genetic material through the act of bacterial conjugation, where the donor bacterium makes a bridge to the receptor bacterium and transfers genetic material. With all these methods of communication, it’s no surprise that the emergence of one case of resistance could potentially obliterate an antibiotic within a couple of years.
Although daunting, antibiotic resistance should not cause panic. The current state of the medical landscape has enough antibiotics in its arsenal to combat most day-to-day infections. Even rare cases of multi-drug resistant superbugs can be treated.
That is not to say that preventative measures can’t be taken. There are some things that anyone can do to limit the spread of antibiotic resistance however. Firstly, always take the antibiotics to term. Many people will stop taking prescribed antibiotics when they start to feel better. This may, however, cause the infection to return with a new resistive vigour. The antibiotics would have killed only the bacteria that are not resistant, and the rebound infection would now be populated with a higher percentage of antibiotic bacteria. Secondly, always take the antibiotics as per the prescription. Neither should you take antibiotics when they are unnecessary. Similarly, overloading your system with antibiotics only benefits the resistive bacteria, which only enhances their proliferation and spread. Antibiotics, in this medical landscape, must be taken with diligence.
Antibiotic abuse is the leading cause of the alarmingly rapid onset of resistance. There are no more failsafe antibiotics on the market, so we must be much more careful about how we use the last treatments we have left. New research is constantly trying to find the answer to this difficult problem. Leading scientists around the world are discovering possible compounds as we speak, and we may soon find a new solution. However, let us not forget the path that took us here and use antibiotics with care.
 News / Right-wing billionaire Peter Thiel gives ‘antichrist’ lecture in Cambridge6 February 2026
News / Right-wing billionaire Peter Thiel gives ‘antichrist’ lecture in Cambridge6 February 2026 News / Cambridge students uncover possible execution pit9 February 2026
News / Cambridge students uncover possible execution pit9 February 2026 Features / From fresher to finalist: how have you evolved at Cambridge?10 February 2026
Features / From fresher to finalist: how have you evolved at Cambridge?10 February 2026 News / Epstein contacted Cambridge academics about research funding6 February 2026
News / Epstein contacted Cambridge academics about research funding6 February 2026 News / Churchill plans for new Archives Centre building10 February 2026
News / Churchill plans for new Archives Centre building10 February 2026









