This Week In COVID-19 Research: 7
Sophie Truepenny takes us through the last week of COVID research, covering perhaps the first piece of good news we’ve seen in this article series: dexamethasone.
This week has seen the continued push for racist and oppressive systems to be rebuilt and has seen a huge new wave of Trans activism following Trump removing discrimination protections based on gender identity, which is likely to have fatal consequences, particularly in the midst of a pandemic.
Closer to home, as the weekend marks the 90th day of the UK lockdown, we bring you this week’s scoop of COVID research from the comeback of staple drug Dexamethasone, to the effects of coronavirus on cancer deaths for the next 10 years.
Policy changes in the UK
The lockdown was brought into place for the benefit of public health, but has undoubtedly damaged the economy; in order to optimise the trade-off, the 2m social distancing rule is to be reviewed this week, the outcome of which - according to Chancellor Rishi Sunak - will “make an enormous difference” to businesses, particularly in the hospitality sector. It is expected that reducing the rule to 1m could allow businesses to break even, generating 70% of the normal revenue rather than 30% at present (at 2m). While WHO suggests at least a 1m distance, the UK government’s scientific advisers state that this increases the risk of infection by up to 10 times.
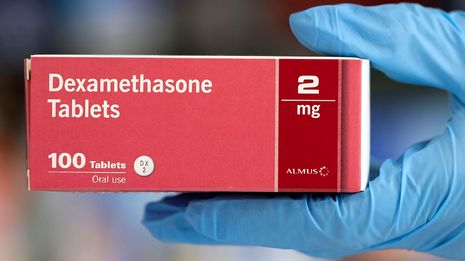
“[Dexamethasone] was shown to reduce deaths by a third in ventilated patients and a fifth in patients receiving oxygen only.”
On increasing public footfall, this week also saw the requirement for face coverings on public transport come into place in England. Though it does not apply to entering shops, the guidance states they should be worn in enclosed public spaces and Manuel Cortes, the general secretary of the TSSA, emphasised that “people must not interpret the use of face coverings as a licence to breach social-distancing measures”. Professor Chris Whitty reiterated this, and ‘urged the public not to buy surgical or medical masks needed for frontline carers, but to rely on scarves or DIY-type masks instead’.
RECOVERY: the dawn of Dexamethasone and the end of Hydroxychloroquine
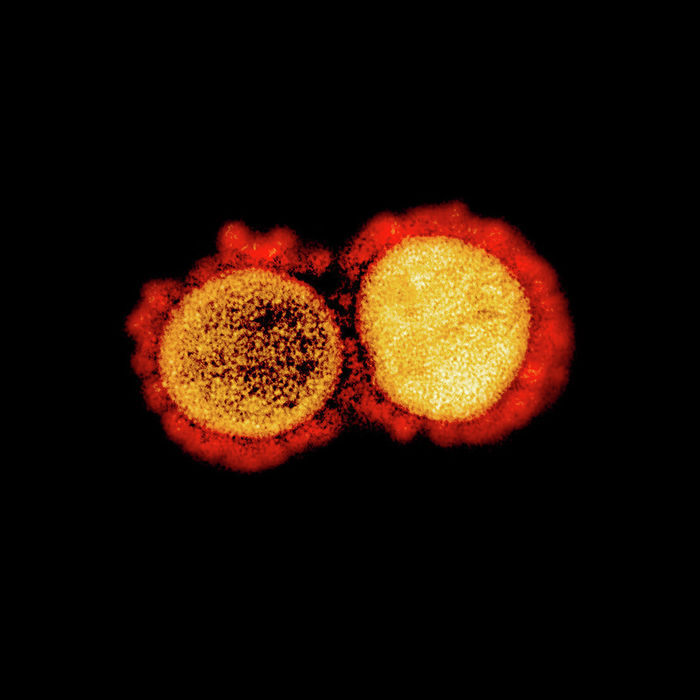
On Tuesday (16th June 2020), the University of Oxford shared a press release announcing the hopeful results of a study launched in March 2020. RECOVERY (standing for Randomised Evaluation of COVid-19 thERapY) was a huge clinical trial spanning 175 NHS hospitals and over 11,500 patients receiving 6 independent treatments. Among others, the treatments studied included Hydroxychloroquine, as first discussed in Varsity Science here and famously taken by President Trump (the use of which has now been halted) and convalescent plasma, which is the blood plasma containing antibodies against the virus collected from donors who have recovered from COVID-19, but the most significant was Dexamethasone.
Dexamethasone is a steroid usually used to treat inflammation, and was given in low doses (6 mg, once daily) to 2104 patients for 10 days. It is the first drug to have been shown to reduce mortality from COVID-19; it’s also very affordable and readily available. “Dexamethasone should now become the standard of care” in severe cases, said Peter Horby, one of the Chief Investigators for the trial and Professor of Emerging Infectious Diseases, University of Oxford. Although there was no benefit to those receiving no respiratory support, it was shown to reduce deaths by a third in ventilated patients and a fifth in patients receiving oxygen only. This, the release quotes, would prevent 1 death “by treatment of 8 ventilated patients or around 25 patients requiring oxygen alone”; it was thereafter immediately authorised in the UK.
What makes me more likely to be hospitalized?
Further to last week’s discussion of increased mortality in BAME (Black, Asian & Minority Ethnic) communities, this paper outlining an analysis across six metropolitan Atlanta hospitals and clinics found characters which put patients at higher risk of requiring hospitalisation. The study of 531 COVID-19 patients showed that “older age, black race, diabetes” as well as “male sex, smoking, and obesity, were independently associated with hospitalization”, and suggested that measures to prevent infection should be emphasised for those in such groups.
“Excess deaths could be a better measure than just ‘coronavirus deaths’, the definition of which varies hugely between countries.”
Disparity in symptoms was also found between hospitalised and non-hospitalised patients – fever and a cough were shared, but shortness of breath was reported more often in hospitalised patients and chills, a headache, loss of smell or taste, or sore throat were more common among non-hospitalised patients. This study confirmed that the loss of sense of taste and smell, without a ‘blocked nose’, is common among COVID-19 patients, and as such COVID-19 should be suspected when these symptoms are present to allow early diagnosis of the disease.
Excess deaths - what do coronavirus death statistics actually mean?
When the lockdown was announced in the UK, it was made clear that all measures were put in place to reduce all types of deaths related to the SARS-CoV-2 outbreak – those caused directly by the disease, but also the indirect deaths due to restricted access to other forms of care such as screenings, surgeries and mental health care. While members of the public have been watching the confirmed deaths due to COVID-19 fall over the last few weeks, the concern over the much higher number of excess deaths globally has risen. For instance, the number of cardiac arrests in recent months has soared. One day in April saw a 10-fold increase in out-of-hospital cardiac arrests in New York City, which across the period studied, showed a 3-fold increase in those needing resuscitation (though it remains unclear whether such patients had tested positive for COVID-19).
Excess deaths is a seemingly simple measure - the number of deaths above the average (over the past 5 years) deaths at this point in the year - but removes the effects of the differences in the number of tests carried out and classification of COVID-19 deaths, and may start to show the indirect deaths the pandemic has caused. Each of these make comparisons between countries almost meaningless, so excess deaths could be a better measure than just ‘coronavirus deaths’, the definition of which varies hugely between countries. This article showed that the UK has reported at least a third more deaths than expected, along with Italy, Spain and Belgium since the beginning of the outbreak in each country.
Cancer and coronavirus
Further to last week’s ‘COVID effects on non-COVID patients’ section, a model this week estimated that the number of excess deaths from colorectal and breast cancers between 2020 and 2030 could be up to 10,000 in the US alone due to the pandemic. This is a result of more avoidance of hospitals due to the fear of catching COVID-19, meaning dissuasion from attending treatments and screenings, which delays diagnoses. There is also fear that the movement restrictions and ‘stay at home’ guidance is shutting labs and reducing the number of clinical trials taking place.
 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / Gov grants £36m to Cambridge supercomputer17 February 2026
News / Gov grants £36m to Cambridge supercomputer17 February 2026 News / CUCA members attend Reform rally in London20 February 2026
News / CUCA members attend Reform rally in London20 February 2026 News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026
News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026