This Week In COVID-19 Research: 2
Maria Izmirlieva distils the last week’s worth of global research on coronavirus-related issues in this instalment of This Week In Covid.
COVID-19 currently seems to dominate every aspect of our lives. Wherever you look (and even if you don’t want to), the airwaves are full of news about scientific developments, government policy changes and the relentless statistics on new infections and fatalities. The rapid pace of development is unprecedented, and it’s almost impossible to keep track of the sheer body of research in this area. At Varsity Science, we aim to go slightly deeper, beyond the mainstream media coverage. Here is a brief summary of some of the noteworthy academic research papers on SARS-CoV-2 from the past week.
A noncompeting pair of human neutralizing antibodies block COVID-19 virus binding to its receptor ACE2
Four different monoclonal antibodies (mAbs) of human origin have recently been isolated from patients recovering from COVID-19 (B38, H4, B5 and H2). The process of COVID-19 infection relies on the SARS-CoV-2 surface S-protein (spike protein) binding to the ACE2 receptors on human cells, thus facilitating entry. B38 and H4 are ‘neutralising’ defensive antibodies as these completely inhibit binding between the receptor binding domain (RBD) of the S-protein and ACE2. Although there was some overlap in activity between B38 and H4, their results showed that these recognise different epitopes (i.e., a specific part of antigen recognised by the immune system). In contrast, B5 and H2 proved to be less effective, with partial or no competition with ACE2 for binding to RBD, respectively. So far, there has been success in therapeutic studies with transgenic mice which possess human ACE2 receptors. The use of these mAbs has successfully reduced viral concentrations in the lungs of infected mice. Such antibodies may offer a promising antiviral treatment for COVID-19 infection in humans in the future.
Find the paper here.
“The triple therapy group had shorter average hospital stays and reported an earlier disappearance of symptoms.”
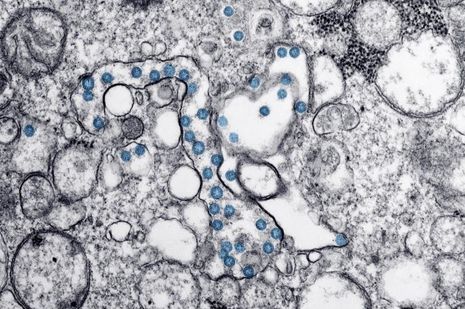
Development of an inactivated vaccine candidate for SARS-CoV-2
Developing an effective vaccine for SARS-CoV-2 remains a critical, yet elusive, target during this public health crisis. Currently, multiple vaccine types including DNA-, RNA-based formulations and purified inactivated virus being developed and trialled. A newly-developed SARS-CoV-2 vaccine candidate, ‘PiCoVacc’ has been found effective in inducing antibody production in mice, rats, and non-human primates (specifically macaques). In the study, 11 representative SARS-CoV-2 strains were collected from hospital patients from China, Italy, Switzerland, the UK and Spain. One of these strains, CN2, was chosen for production of the vaccine itself, whereas the other 10 strains were used as preclinical challenge strains. Authors report that in experiments on mice, PiCoVacc could elicit a tenfold increase in antibody levels compared to the antibody levels in serum of patients recovering from COVID-19. Also, the inactivated vaccine successfully neutralised all 10 challenge strains when the mice were infected. In macaques, those who had received the larger dosage (6-micrograms) showed complete protection, whereas those given 3-micrograms showed partial protection. Notably, PiCoVacc did not lead to the antibody-dependent enhancement (ADE) phenomenon, which has been cited as a concern in vaccine development. These data support the move of PiCoVacc into clinical development, with human trials expected to begin later this year.
Find the paper here.
Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial
In the interim before specific targeted therapies for SARS-CoV-2 are developed, scientists look to find COVID-19 treatments by repurposing drugs already approved for other infections. In a study recently published in the Lancet, a combination of interferon beta-1b, lopinavir-ritonavir and ribavirin may offer a promising treatment for patients with mild to moderate cases of COVID-19. These three drugs are currently approved for treating other illnesses: interferon beta-1b for multiple sclerosis, lopinavir-ritonavir as an anti-retroviral treatment in HIV, and ribavirin for hepatitis C. More than 120 patients in six hospitals in Hong Kong were enrolled in the trial. Their results indicated that the patients treated with the triple antiviral treatment had a significantly shorter median time from the start of the study to a negative test (7 days), compared to those treated with only lopinavir-ritonavir (12 days). Also, the triple therapy group had shorter average hospital stays and reported an earlier disappearance of symptoms. However, further testing will be required since the study sample size was very limited and the study was not ‘blinded’, meaning both doctors and participants knew which drugs were given.
Find the paper here.
Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin–angiotensin–aldosterone inhibitors
Epidemiological observations have indicated that men are not only more likely to test positive for COVID-19, but also have a higher risk of complications and an increased mortality rate. According to a study published in the European Heart Journal, men have higher concentrations of angiotensin-converting enzyme 2 (ACE2), which may explain this higher incidence and fatality. As part of the study, samples of over 3500 heart failure patients from 11 European countries were collected. ACE2 is a critical receptor on cells, which binds to the viral surface S-protein, mediating entry into the cell and allowing infection. ACE2 is widely distributed in the tissues, including, but not limited to, the lungs, kidneys, heart and testes. In men, there is tissue-specific transcriptional regulation of ACE2, which may explain these elevated ACE2 protein concentrations, and ultimately, increased vulnerability. The study also revealed that ACE inhibitors and angiotensin II receptor blockers (ARBs) did not lead to increased ACE2 concentration. This fact should be reassuring to people concerned that taking these commonly-used cardiovascular drugs may be putting them at higher risk of COVID-19 complications.
Find the paper here.
 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / Gov grants £36m to Cambridge supercomputer17 February 2026
News / Gov grants £36m to Cambridge supercomputer17 February 2026 News / CUCA members attend Reform rally in London20 February 2026
News / CUCA members attend Reform rally in London20 February 2026 News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026
News / Union speakers condemn ‘hateful’ Katie Hopkins speech14 February 2026 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026