Harvard diabetes breakthrough
Trinity graduate Douglas Melton makes a huge step towards developing a cure
For over 250,000 people diagnosed with type I diabetes in the UK, a cure is on the horizon.
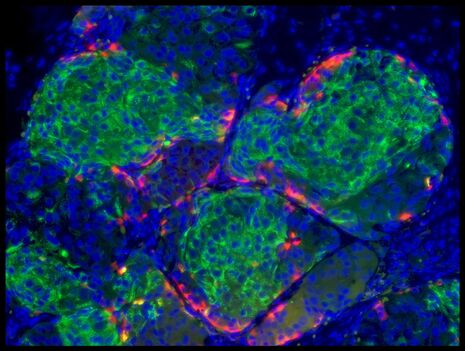
Douglas Melton, Harvard’s Xander University Professor and co-director of the Harvard Stem Cell Institute, has with his team of colleagues discovered the complex series of steps that program stem cells into insulin-producing beta cells. Excitingly, they cured diabetic mice by transplanting in beta cells derived from human stem cells.
Type I diabetics are afflicted with an autoimmune response that kills beta cells. This leads to an inability to produce insulin, the hormone that facilitates glucose absorption from the blood into muscle and tissue.
This advance could allow stem cell-derived beta cells to replace the battery of insulin injections regimented into the daily life of a type I diabetic, a treatment method in which advances have stagnated. While the options of insulins available have diversified and moved from purified animal proteins to human insulin from a cloned insulin gene, scientists have so far been unable to move beyond the injection. “This is a kind of life support for diabetics. It doesn’t cure the disease and leads to devastating and very costly complications”, Melton explains.
“We are very excited about this”, says Melton, a graduate of Trinity College. “It provides for type I diabetics, in my view, half of the solution to their problem”. The other half of the problem lies in the autoimmune response and protecting newly introduced beta cells from attack – a challenge that Melton is confident can be overcome through the use of an immunosuppressant drug, or by an encapsulation device. Advances on such a device include the development of seaweed-derived gelatinous capsules, pioneered by MIT bioengineer Daniel Anderson, which are capable of protecting clusters of beta cells.
Although only half the problem is solved, Melton’s work may be life-changing for millions of diabetics worldwide.
 News / Uni members slam ‘totalitarian’ recommendation to stop vet course 15 January 2026
News / Uni members slam ‘totalitarian’ recommendation to stop vet course 15 January 2026 Science / Why smart students keep failing to quit smoking15 January 2026
Science / Why smart students keep failing to quit smoking15 January 2026 Interviews / The Cambridge Cupid: what’s the secret to a great date?14 January 2026
Interviews / The Cambridge Cupid: what’s the secret to a great date?14 January 2026 Comment / Will the town and gown divide ever truly be resolved?12 January 2026
Comment / Will the town and gown divide ever truly be resolved?12 January 2026 News / Cambridge bus strikes continue into new year16 January 2026
News / Cambridge bus strikes continue into new year16 January 2026








